Scientists tell that ALS is a disease striking upper motor neurons, which in a cascade effect, affects the lower motor neurons and muscles. Yet this does not match the patient's experience.
 For them, symptoms often start with weakness, unreliability, and thinning of the thumb or calf, and with time the disease progresses to other (skeletal) muscles.
For them, symptoms often start with weakness, unreliability, and thinning of the thumb or calf, and with time the disease progresses to other (skeletal) muscles.
Scientific approaches are focussing on healing upper motor neurons (with a complete lack of success, which hints that we understand nearly nothing in this area) or replacing them (there are still no clinical studies).
For most scientists, it would be meaningless to try to replace muscles in ALS patients, as the upper motor neurons are dead (despite evidence they are not) new muscles would never be usable and therefore waste and die quickly.
And anyway grafting muscles on neuromuscular junctions is an extraordinarily difficult problem.
Yet there are contrarians: Scientists have recently unveiled an approach to address the devastating effects of amyotrophic lateral sclerosis (ALS), on muscle weakness. Their research introduces a novel technique involving a combination of grafted replacement motor neurons and optical nerve stimulation.
By employing a two-pronged strategy—grafting modified motor neurons and using light-based nerve stimulation—the researchers managed to rejuvenate muscle function, marking a tiny step toward devising effective therapies for ALS.
Led by Dr. Barney Bryson, the team of scientists had shown potential in restoring muscle denervation in a mouse model by utilizing optical nerve stimulation. This method hinged on grafting replacement motor neurons that were engineered to be light-sensitive, enabling their activation through an external light source.
In this latest study, the initial objective was to ensure the survival of donor motor neurons during the grafting process, overcoming potential immune system rejection. After determining that conventional immunosuppressive drugs were not viable for ALS mice, the researchers experimented with a specific antibody known as H57-597, which successfully prevented graft rejection and began reconnecting nerves to target muscles. Despite these positive outcomes, the force generated by muscle contractions was relatively weak, prompting the team to further refine their strategy.
Recognizing that neuromuscular junctions—the connection points between nerves and muscles—are influenced by regular stimulation, the scientists introduced a wireless optical stimulation system to enforce consistent muscle contractions for an hour each day. Astonishingly, after 21 days of this optical stimulation training, the mice exhibited an astonishing 13-fold enhancement in muscle contraction force. That would be nearly three years of rehabilitation therapy in humans.
These findings carry immense significance, demonstrating that even in the advanced stages of ALS, affected muscles remain amenable to reinnervation by healthy replacement motor neurons.
The strategy suggests the feasibility of a treatment that could potentially be universally applied to all ALS patients regardless of the kind of ALS they have (familial or sporadic).
More significantly, it tells that the model of ALS progression which was derived from stroke ~150 years ago and mostly never questioned since all these decades, is simply wrong.
However, significant challenges remain before this approach can transition to clinical use. Subsequent studies are necessary to confirm the efficacy of the grafting procedure with human motor neurons and to evaluate whether it can genuinely enhance patients' quality of life. Furthermore, the technique's applicability to other forms of MND, particularly those with longer life expectancies, must be investigated to ascertain its long-term effectiveness.
In conclusion, the study's senior author, Linda Greensmith, emphasizes that the findings underline the robustness of replacing motor neurons to reinnervate muscles even in advanced ALS stages. Should this approach successfully translate to ALS patients, it holds the potential to revolutionize treatment by employing a single type of motor neuron for various muscles, simplifying the therapy and making it more widely accessible. The introduction of this approach could be a game-changer in the ongoing battle against ALS and other related neuromuscular conditions.
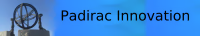
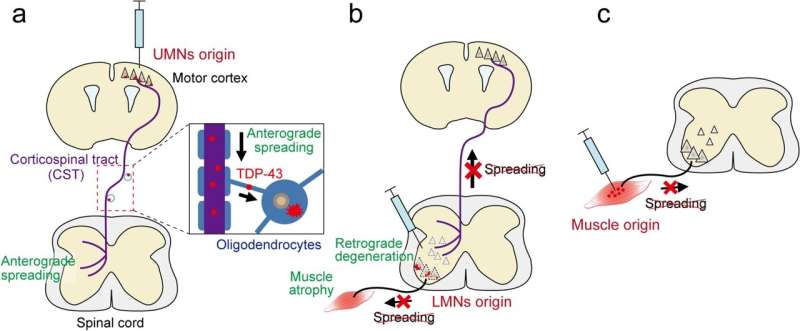 Les auteurs ont établi de nouveaux modèles de SLA de souris qui induisaient initialement des inclusions de TDP-43 mutant dans des types neuronaux ou cellulaires spécifiques dans les circuits moteurs, et ils ont étudié si le TDP-43 et les processus pathologiques pertinents se propageaient à travers les connexions neuronales ou cellulaires.
Les auteurs ont établi de nouveaux modèles de SLA de souris qui induisaient initialement des inclusions de TDP-43 mutant dans des types neuronaux ou cellulaires spécifiques dans les circuits moteurs, et ils ont étudié si le TDP-43 et les processus pathologiques pertinents se propageaient à travers les connexions neuronales ou cellulaires. Tsuboguchi et al., Acta Neuropathologica 2023.
Tsuboguchi et al., Acta Neuropathologica 2023.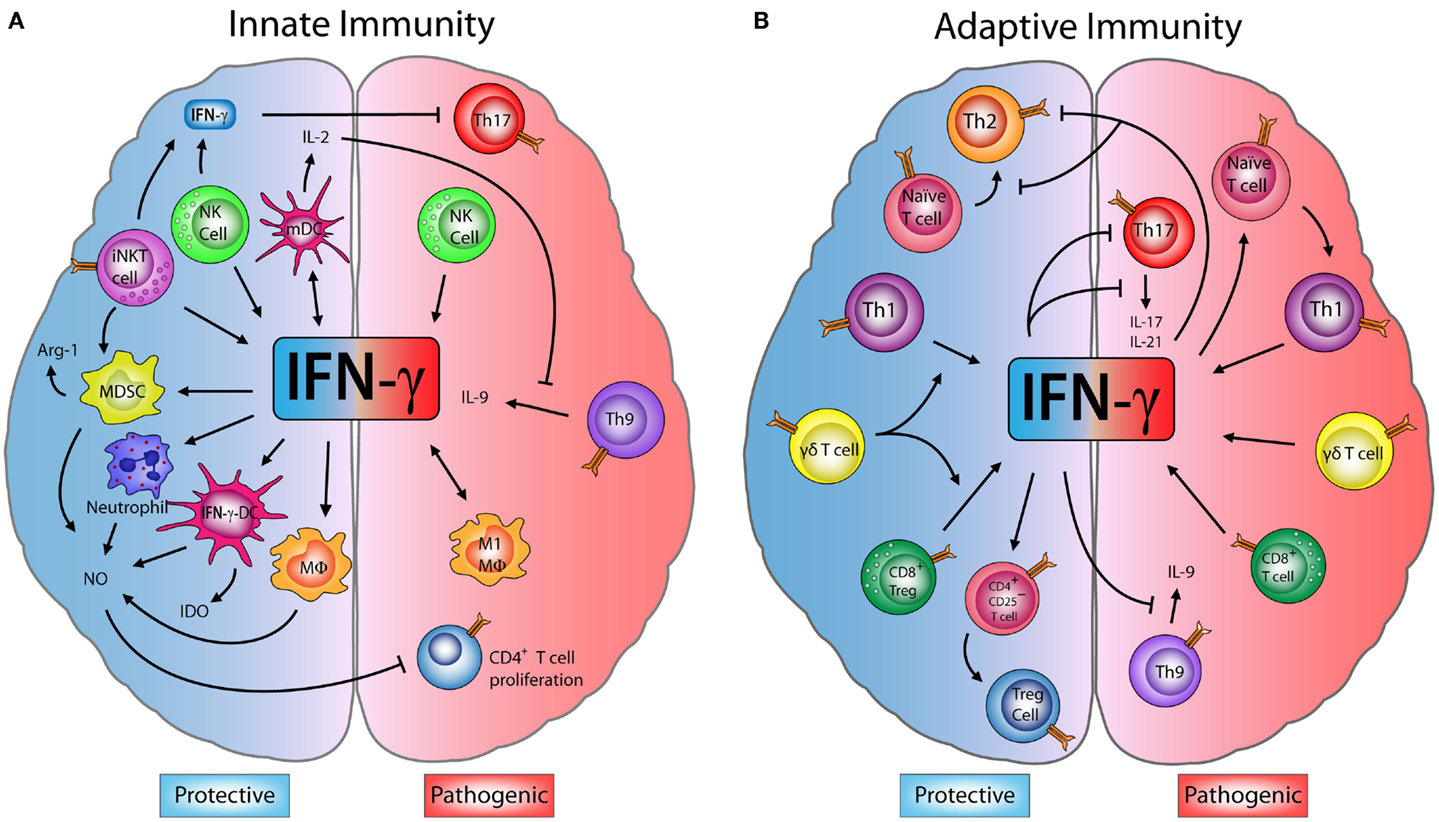
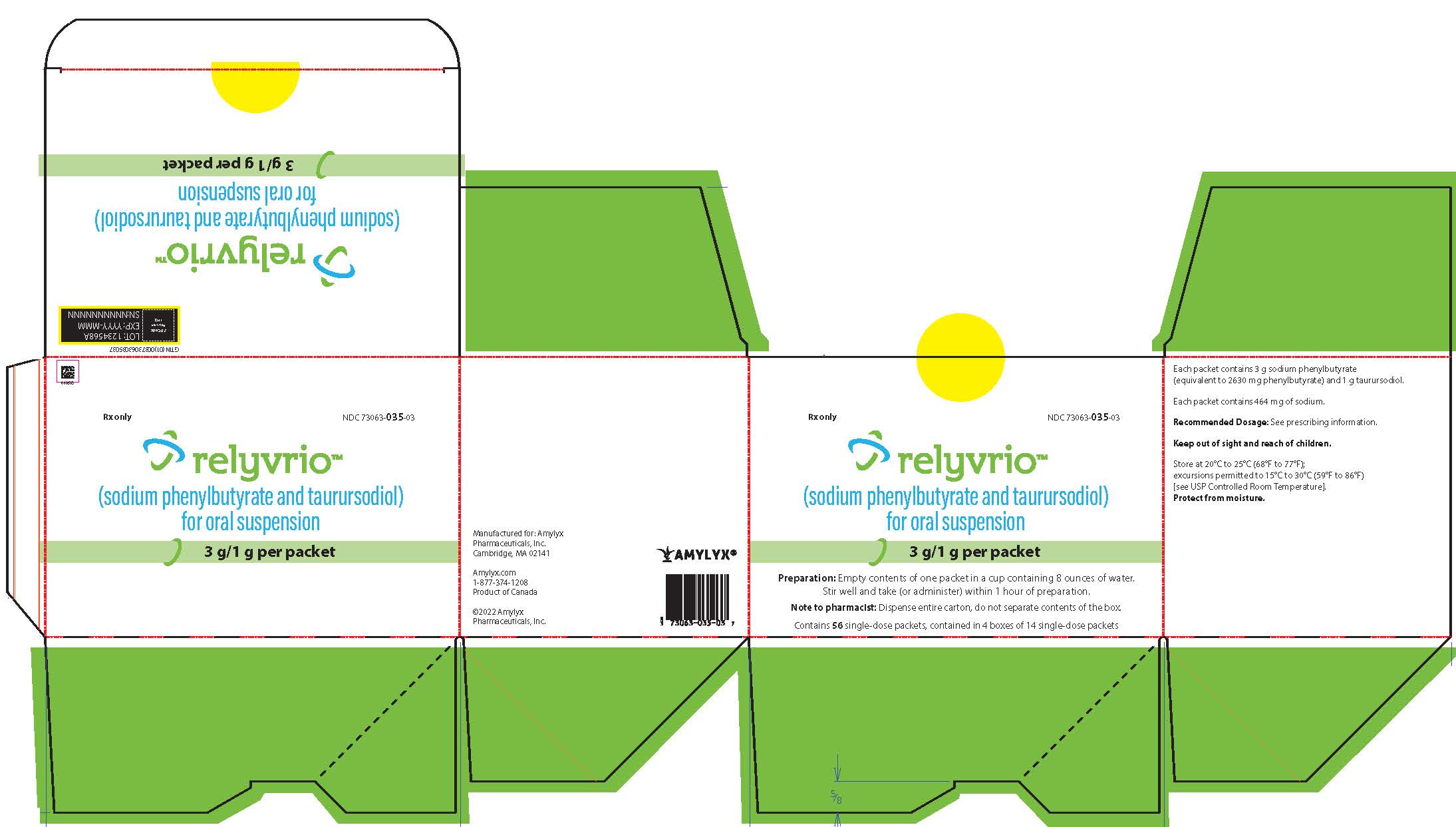 La FDA et l'agence Européenne des médicaments ont exprimés de nombreux doutes sur l'efficacité de ce médicament au cours de l'essai CENTAUR.
Ces doutes concernent l'exclusion d'un certain nombre d'évènements défavorables lors de l'analyse statistique, ainsi que le fait que certains patients ont aussi reçu du Riluzole et de l'Edaravone.
En particulier il y a plus de patients ayant reçu de l'Edaravone dans la branche contrôle que dans la branche traitement, or certains scientifiques et agences du médicament pensent que l'Edaravone a un effet négatif sur l'évolution de la maladie. Certains médecins ont également attribué les "bons" résultats au TUDCA.
Au final à 24 mois il n'y a pas d'amélioration de la survie.
La FDA et l'agence Européenne des médicaments ont exprimés de nombreux doutes sur l'efficacité de ce médicament au cours de l'essai CENTAUR.
Ces doutes concernent l'exclusion d'un certain nombre d'évènements défavorables lors de l'analyse statistique, ainsi que le fait que certains patients ont aussi reçu du Riluzole et de l'Edaravone.
En particulier il y a plus de patients ayant reçu de l'Edaravone dans la branche contrôle que dans la branche traitement, or certains scientifiques et agences du médicament pensent que l'Edaravone a un effet négatif sur l'évolution de la maladie. Certains médecins ont également attribué les "bons" résultats au TUDCA.
Au final à 24 mois il n'y a pas d'amélioration de la survie.
 In the case of ALS, the clusters of TDP-43 are also located in the cytosol, i.e. where the proteins are produced, before being folded up in the ER and then sent to their place of use by the Golgi apparatus. After shipment, TDP-43 should be in the nucleus.
In the case of ALS, the clusters of TDP-43 are also located in the cytosol, i.e. where the proteins are produced, before being folded up in the ER and then sent to their place of use by the Golgi apparatus. After shipment, TDP-43 should be in the nucleus. Des preuves cliniques et épidémiologiques établissent un lien entre les altérations métaboliques et l'apparition et la progression de la sclérose latérale amyotrophique. Ces défauts métaboliques précèdent les symptômes moteurs, ce qui suggére que ces défauts sont au moins en partie à l'origine de la SLA.
Des preuves cliniques et épidémiologiques établissent un lien entre les altérations métaboliques et l'apparition et la progression de la sclérose latérale amyotrophique. Ces défauts métaboliques précèdent les symptômes moteurs, ce qui suggére que ces défauts sont au moins en partie à l'origine de la SLA. Des scientifiques se sont demandé quel était l'impact de l'exposition aux stéroïdes endogènes et synthétiques chez les patientes atteinte de la SLA. Ils ont comparé cet impact à celui d'un groupe comparable mais ne souffrant pas de la SLA.
Des scientifiques se sont demandé quel était l'impact de l'exposition aux stéroïdes endogènes et synthétiques chez les patientes atteinte de la SLA. Ils ont comparé cet impact à celui d'un groupe comparable mais ne souffrant pas de la SLA. The authors initially hypothesized that activation of the inhibitory co-receptor PD-1 by recombinant PD-L1 would be anti-inflammatory. However, recombinant PD-L1 ligand and recombinant PD-1 receptor were strongly pro-inflammatory.
Then they abandoned the PD-L1 strategy and chose a strategy with dimethyl fumarate (DMF), a drug approved against two autoimmune diseases, multiple sclerosis and psoriasis, and the cGAS- STING H-151 involved in autoimmunity.
The authors initially hypothesized that activation of the inhibitory co-receptor PD-1 by recombinant PD-L1 would be anti-inflammatory. However, recombinant PD-L1 ligand and recombinant PD-1 receptor were strongly pro-inflammatory.
Then they abandoned the PD-L1 strategy and chose a strategy with dimethyl fumarate (DMF), a drug approved against two autoimmune diseases, multiple sclerosis and psoriasis, and the cGAS- STING H-151 involved in autoimmunity. Les inhibiteurs classiques de mTOR tels que la rapamycine ou la metformine peuvent améliorer les dommages aux neurones. Une autre approche importante pour lutter contre les ND est l'utilisation de produits/composés naturels comprenant des antioxydants, des flavonoïdes, des polyphénols et des acides gras polyinsaturés (PUFA). Diverses études ces dernières années ont montré les effets bénéfiques des acides gras poly insaturés (AGPI) oméga-3 à travers divers mécanismes dont des effets anti-inflammatoires. Les acides gras oméga-3 les mieux étudiés sont l'acide docosahexaénoïque (DHA), l'acide eicosapentaénoïque (EPA) et l'acide α-linolénique (ALA).
Les inhibiteurs classiques de mTOR tels que la rapamycine ou la metformine peuvent améliorer les dommages aux neurones. Une autre approche importante pour lutter contre les ND est l'utilisation de produits/composés naturels comprenant des antioxydants, des flavonoïdes, des polyphénols et des acides gras polyinsaturés (PUFA). Diverses études ces dernières années ont montré les effets bénéfiques des acides gras poly insaturés (AGPI) oméga-3 à travers divers mécanismes dont des effets anti-inflammatoires. Les acides gras oméga-3 les mieux étudiés sont l'acide docosahexaénoïque (DHA), l'acide eicosapentaénoïque (EPA) et l'acide α-linolénique (ALA).